Diabetes & Vision Loss
Diabetes is a chronic health condition affecting how the body produces or uses insulin (the hormone that regulates sugar levels). Over time, uncontrolled diabetes can cause severe health problems, including vision loss.
Diabetic retinopathy is an eye disease that can develop because of diabetes. The condition can be detected with a comprehensive eye exam and eye health monitored with regular diabetic eye exams.
Learn about the stages of diabetic retinopathy and what you can do to protect your eyesight.
What Is Diabetic Retinopathy?
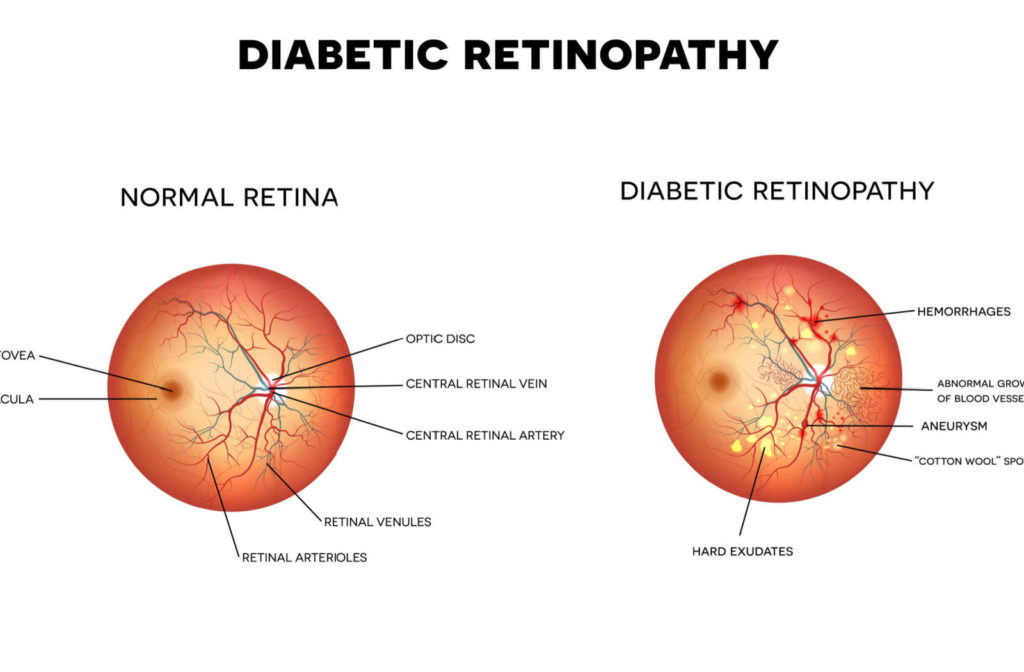
Diabetic retinopathy occurs when too much sugar in the blood damages cells in the body, including small blood vessels in the retina. The retina is a light-sensitive tissue layer at the back of the eye. It can detect color and light intensity, processing visual information to send to the brain through the optic nerve.
The risk of developing diabetic retinopathy increases the longer a person has diabetes. The condition usually affects both eyes and can lead to blindness if untreated.
When blood sugar levels are controlled, treatment can reverse some vision problems associated with diabetes. For example, when high blood sugar causes fluid to accumulate in the eye, the buildup can change the lens’ shape and affect focusing ability. Receiving treatment and reducing blood sugar levels can help the lens return to normal shape and improve vision.
Common symptoms of diabetic retinopathy include:
- Blurred vision
- An empty/dark spot in central vision
- Increased floaters & spots
- Poor night vision
The 4 Stages
Health problems caused by diabetes are progressive and worsen over time. Diabetic retinopathy is classified into 2 types and 4 stages to describe the disease progression.
The early stages are nonproliferative, referring to the absence or control over abnormal blood vessel growth. The later stages are proliferative, which refers to the rapid growth of abnormal blood vessels. The abnormal growth increases with higher blood sugar levels.
Stage 1: Mild Nonproliferative Diabetic Retinopathy
The earliest stage of the disease typically includes mild symptoms. There may be swelling in retinal blood vessels, known as microaneurysms. The swelling can cause the blood vessels to leak or bleed into the retina area.
The leaking fluid can cause the macula to swell. The macula is an oval-shaped tissue (located in the middle of the retina) crucial for color and central vision. The condition known as macular edema can cause blurry or distorted central vision and dull color perception.
Stage 2: Moderate Nonproliferative Diabetic Retinopathy
In the second stage, blood vessel swelling increases and can block blood flow to the retina. Without adequate blood flow, the retina cannot receive nourishment. As a result, fluids accumulate, and leaking can worsen, increasing the risk of macular degeneration.
Stage 3: Severe Nonproliferative Diabetic Retinopathy
As the disease progresses into the third stage, symptoms and eye health risks can increase. More swelling and blockage can significantly decrease blood flow to the retina.
The body receives signals to grow new blood vessels in response to the lack of blood flow. Unfortunately, the newer blood vessels can develop abnormally, leading to the proliferative stage of the disease.
Stage 4: Proliferative Diabetic Retinopathy
The most advanced stage of the disease increases risks for retina and eye damage. New, abnormal blood vessels form in the retina. The abnormal blood vessels are fragile and have a higher risk of leaking fluids or bleeding.
Proliferative diabetic retinopathy can cause multiple vision symptoms and lead to blindness.
Diagnosing Diabetic Retinopathy
Optometrists assess eye health during comprehensive eye exams. Regular eye exams can detect changes to eye structures, including the retina, macula, and blood vessels, to diagnose diabetic eye disease.
Dilated eye exams are commonly used to examine structures at the back of the eye, including the retina and optic nerve. Other evaluations that can help diagnose diabetic retinopathy include:
- Depth perception
- Eye muscle movement
- Peripheral vision
- Visual acuity
After receiving a diagnosis, diabetic eye exams are crucial for monitoring eye health and implementing treatment when appropriate.
Treating Diabetic Retinopathy
Diabetic retinopathy can lead to irreversible vision loss. Fortunately, there are treatment options that can help preserve eyesight. Patients have the greatest chance of success in the nonproliferative stages, so early detection and treatment are crucial.
Managing diabetes by controlling blood sugar levels can be the most effective way to prevent severe diabetic eye disease. Some patients may manage diabetes with medication, diet, and physical activity.
When symptoms present or eye damage increases, some treatment options include:
- Eye medication: Steroid injections can prevent the formation of abnormal blood vessels. Anti-VEGF injections can help reduce macula swelling.
- Laser surgery: Photocoagulation is performed to prevent the development of abnormal blood vessels and seal leaking blood vessels. The surgery can help reduce swelling and improve blood flow.
- Vitrectomy: When eye damage causes retina scarring or significant leakage, a vitrectomy is performed to remove the vitreous and excess fluid. Then, the retina is repaired, and an artificial (silicone) vitreous is inserted to help improve vision.
Check Your Eye Health Today
1 in 5 American adults have undiagnosed diabetes. Regular eye exams can help detect eye problems before symptoms become severe. It’s also crucial to have regular diabetic eye exams if you know you’re at risk of developing a diabetic eye disease, including diabetic retinopathy. We want to help you protect your sight. With over 30 years of experience, trust Seal Beach Eyes to provide compassionate eye care for you and your family. Contact us to learn more about our services, or book an appointment today!